 Anytime you workout in a gym, you are exposed to a plethora of germs. Right now, there is a huge flu pandemic going on, so there is good reason to protect yourself. Follow these rules to save yourself from being sick:
Anytime you workout in a gym, you are exposed to a plethora of germs. Right now, there is a huge flu pandemic going on, so there is good reason to protect yourself. Follow these rules to save yourself from being sick:
An estimated 70% of ACL injuries do not involve contact, and may be from a simple misstep. How can you help avoid these injuries and stay off the sidelines?
 Athletes who have suffered an ACL injury are at increased risk of developing arthritis later on in life, even if they have surgery for the injury. It
Athletes who have suffered an ACL injury are at increased risk of developing arthritis later on in life, even if they have surgery for the injury. It
 In this article CoreFit focuses on Orthobiologics. Naturally formed substances, Orthobiologics in the form of matrix, growth factors and stem cells, can be injected into the injury site to speed up recovery. I break down the way these substances work within your body.
In this article CoreFit focuses on Orthobiologics. Naturally formed substances, Orthobiologics in the form of matrix, growth factors and stem cells, can be injected into the injury site to speed up recovery. I break down the way these substances work within your body.
CoreFit Focus: Orthobiologics
Orthobiologics are substances that orthopaedic surgeons use to help injuries heal more quickly. They are used to improve the healing of broken bones and injured muscles, tendons, and ligaments. These products are made from substances that are naturally found in your body. When they are used in higher concentrations, they may help speed up the healing process.
Healing Process:
When you injure a bone, muscle, or tendon, there is bleeding into the injured area. This bleeding is the foundation for the healing response. It provides a way for healing factors to reach the injury site.
In addition to bleeding, there are three factors necessary for healing. All three are orthobiologic substances. They include:
Matrix (Conductive Material)

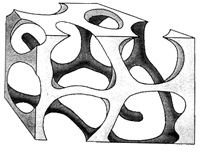
The matrix, or conductive material, provides housing for stem cells while they grow into mature cells. If stem cells do not have a house to grow in, they cannot develop into repair cells that can heal bone, muscle, tendon, or cartilage.
When someone breaks or fractures a bone, the healing process begins. As long as most of the bony substance is not lost, stem cells should be able to make new bone and promote healing. If, however, a significant portion of the broken bone is lost, a large gap may result. This can happen if the bone crumbled, or broke into several pieces and went through the skin.
Under these circumstances, the gap must be filled with matrix, or conductive material, to house stem cells. There are several types of substances that may be used for this purpose.
Bone grafts are often used as matrix material. There are two types of bone grafts.
Autograft. A bone graft can be obtained from the patient. This type of graft is called an autograft. Many different bones can be used to supply the graft. Grafts are most commonly taken from the iliac crest, which is part of the pelvis.
Harvesting a bone graft requires an additional incision during the operation to treat the injury. This makes the surgery take longer and can cause increased pain or risk of infection after the operation. Although autografts have been used with good results, some people may experience pain at the donor site for some time.

Allograft. One alternative to taking the bone graft from the patient is called an allograft, which is cadaver bone. An allograft is typically acquired through a bone bank. Like other organs, bone tissue can be donated upon death.
The use of allografts has grown because it avoids the risk of pain at the donor site. There are risks and benefits for both types of bone grafts, which your surgeon will discuss with you.
Man-made materials, such as calcium phosphate, may also be used to fill a large void between bone ends. When treated properly, calcium phosphate can form material that closely resembles bone. It contains holes that are the right size for stem cells to enter and develop into mature cells.
Both calcium phosphate and cadaver bone eliminate the pain and other risks involved with having extra surgery to harvest an autograft.
Growth factors are found inside bone in low concentrations, and in other parts of your body. They can be produced in higher concentrations through genetic engineering.
A lot of work is being done using genetic engineering to help with medical problems. Genetic engineering has made great improvements in making bone heal faster and better.
Genetic engineering can produce large quantities of a needed element in its pure form. During the genetic engineering process, signals inside a cell are altered in order to change the cell’s function. To help with bone healing, cells can be turned into factories that produce growth factor proteins.
Growth factor proteins play an important role in the healing process. They call stem cells to the injury site. This is called chemoattraction. The stem cells are drawn to the injured area where they develop into “repair” cells.
Chemoattraction works only when there is a good blood supply around the injured area. If there is not good blood flow, the proteins cannot attract stem cells, or provide them with a way to travel to the area where they are needed.
Many types of proteins aid in bone healing and can be produced with genetic engineering. The most powerful of these are bone morphogenetic proteins (BMPs). These synthetic proteins also help with muscle, tendon, and cartilage healing. Discovered during the 1960s, BMPs today are produced in large enough quantities to effectively speed the healing of damaged bone, especially in fractures that have a difficult time healing.
Of all the types of cells, stem cells have the greatest potential for promoting healing. As discussed above, stem cells are immature cells that are influenced by their surroundings. When brought to an injury site, a stem cell can develop into the kind of cell needed to help in healing – bone, muscle, ligament, and cartilage.

Because of the healing capabilities of stem cells, doctors have developed ways to bring stem cells to an injury site faster and in greater numbers. The first step in this process is to retrieve the stem cells. This can be done by harvesting them from the patient, or through a stem cell donor program.
There are many sources of stem cells in the human body. The most important source is bone marrow. Bone marrow is located in the centers of long bones, such as the bones in your arms, forearms, thighs, and legs. The pelvic bone contains the highest concentration of stem cells. Therefore, the bone marrow in your pelvic bone is the most common source for harvesting stem cells.
The doctor draws the stem cells out of the bone marrow with a needle, in a similar way that blood is drawn from your arm for tests. An orthopaedic surgeon then inserts this large supply of stem cells into the injury site. This eliminates the time it would take for the stem cells to reach the injury on their own and delivers them in a higher concentration, which speeds the healing process.
Orthopaedic surgeons can also use donor stem cells to promote healing. In much the same way that blood transfusions help millions of patients each year, stem cells taken from donors after they pass away help millions of orthopaedic patients. When these cells are harvested, they are treated so that they will not create an immune or allergic reaction in the patient.
 CoreFit isn’t just about fitness, it’s about life. Even athletes (who are not the typical drinker) like to have fun! Here’s the survival basics for a great NYE.
CoreFit isn’t just about fitness, it’s about life. Even athletes (who are not the typical drinker) like to have fun! Here’s the survival basics for a great NYE.
 At a meeting of The American Society of Hematology on Sunday, researchers from the University of Pennsylvania presented their findings on what very well could be a genetic therapy cure for cancer.
At a meeting of The American Society of Hematology on Sunday, researchers from the University of Pennsylvania presented their findings on what very well could be a genetic therapy cure for cancer.
The concept utilizes a disabled form of HIV that genetically alter the patients own T cells to attack malignant B cells. Providing the patient with something better than a drug–a lasting way for the immune system to fight cancer.
University of Pennsylvania researchers developed the experimental treatment that has been tested on 12 patients,
 In America, the average athlete has been trained to think that an ibuprofen will heal any injury. In fact, 70 percent of
In America, the average athlete has been trained to think that an ibuprofen will heal any injury. In fact, 70 percent of

CHICAGO: Breast cancer screenings are again in the news as the Radiological Society of North America (RSNA, meeting in Chicago this week) claims that the guidelines set forth by the U.S. Preventive Services Task Force — an independent medical panel with federal support–could discourage some women from being screened. The Radiological Society obviously has an interest (some might say conflict of interest) in promoting its own procedures that sometimes cause false-positive cancer diagnosis and over-treatment.
The RSNA looked at rates of mammograms from women 65yrs and older on Medicare. The rates of screenings inched up 1% between 2005 and 2009, but dropped as soon as the U.S. Preventative Services Task Force released their recommendation.
The claim that increased screening leads to decreased mortality is both confusing and controversial simply because there are many cases of screenings which result in early detection and misdiagnosis. They catch cancer that has to be biopsied and in many cases turns out to be malignant, but this doesn’t take into account the fact that no one knows which cancers will be fatal or not.
The problem, the panel said, is that for women younger than 50, the benefits of mammograms may not outweigh the risks. Those include “false-positive” results that lead to needless invasive tests and anxiety (which are more common in women younger than 50), and over-treatment of early breast tumors that would never have progressed.
Proudly powered by WordPress
Theme: Esquire by Matthew Buchanan.